What started out as a novel virus isolated to the city of Wuhan, China, has become a global pandemic of a scale that almost none of us have ever lived through. Predictably, side effects of a pandemic of this magnitude include hysteria and anxiety, both valid responses given the circumstances. Personally, my coping mechanisms are mediocre at best and include completely disassociating and or refreshing my news app every four minutes.
One thing that always helps, though, is hard facts from medical professionals. We spoke with GP Fletcher Charlton on everything you need to know from a health perspective on COVID-19.
What is your advice to those experiencing high levels of anxiety around catching the virus?
It certainly is a scary time with this virus sweeping across the world – it is by far the biggest challenge this generation has faced. Based on data COVID-19 is much more transmissible than the flu and also carries a mortality rate 12-23x that of the flu.
That being said, for the vast majority of people this virus will represent a mild to moderate flu-like illness, however a minority (especially the older populations and those with chronic conditions) will become sicker and need hospital and even life support through incubation and ventilation. Because so many people are predicted to catch the virus, the numbers of people who will need help from the hospital will also be very high and at the predicted rate of growth of community transmission we will not have enough life support machines to care for people.
Until we are able to identify a useful treatment or get a successful vaccination, we need to try and slow the spread of COVID-19 over time so that hospitals can cope with the increased patients.
All this aside, there are some positives to take away from this pandemic: It has been an amazing response from the global community with many countries working together. Being the first pandemic of the information and social media age - there has been rapid sharing of evidence and data to allow us to make informed decisions about how to manage this outbreak. The world’s leading medical journals (The Lancet and JAMA) have allowed free access to evidence surrounding COVID-19. It is also important to get correct information from reputable sources. There is some easy to understand evidence-based information available through the Australian Government, but also the World Health Organisation.
What are the tangible steps we can take to avoid catching the virus?
Social Distancing, Social Distancing, Social Distancing! The virus is primarily spread by droplet transmission. These droplets get passed around through touching and then infect people when they make contact with the mucosal surfaces (eg. eyes, mouth, nose). This is why there is advice on washing your hands with hand sanitiser (or even better soap and water) and trying to avoid touching your face. If you are coughing and sneezing you may aerosolise the virus, which can infect people without touching them. For this reason, it’s important to wear a mask to protect others if you are coughing and sneezing. Unfortunately, it does not seem that wearing a mask will make you any less likely to catch the disease and so it is not recommended if you are well.
For people not in financial positions to self-isolate, how can we best protect ourselves?
From a medical point of view, I don’t think you need to worry about isolating yourself if you remain well and do not have medical conditions that put you at higher risk – but we do need to practice social distancing. If you become unwell, you should isolate yourself and chat to your GP about when it is safe to return to work – Again the best information is on the Australian Government health website.
For everybody, social distancing is the best way to protect yourself and those around you– this involves limiting unnecessary interactions where hand to hand and face to face spread of the virus can occur. In particular we should try to limit interaction with the people more likely to be affected - that is older populations and those with chronic health conditions. Practicing good hand hygiene especially washing hands before and after high-risk settings (grocery shopping – try to minimise too much touching a putting back of items) and using tap payments over handling cash.
A good night sleep, exercise and sunshine are powerful protectors of the immune system. When you get run down, worn out and over-tired you are much more likely to catch any virus. Stop smoking as well – this is hugely important. Smoking is very expensive when money might be short and greatly increases the chances of a lethal response to the coronavirus. Please chat to your GP about quitting – we can more than double your likelihood of successfully quitting.
Do you have any predictions for how we might get COVID-19 under control?
The best evidence and expert opinion suggests social distancing can slow and perhaps even limit the spread of COVID-19 – this is most important and is going to take a massive and diligent effort on the part of the community. We are hopeful that we may uncover some treatments that improve survival. There is currently some weak evidence for an antiviral medication though further data is required and mass supply of this medication will be another issue. There are also many teams working concurrently on vaccinations.
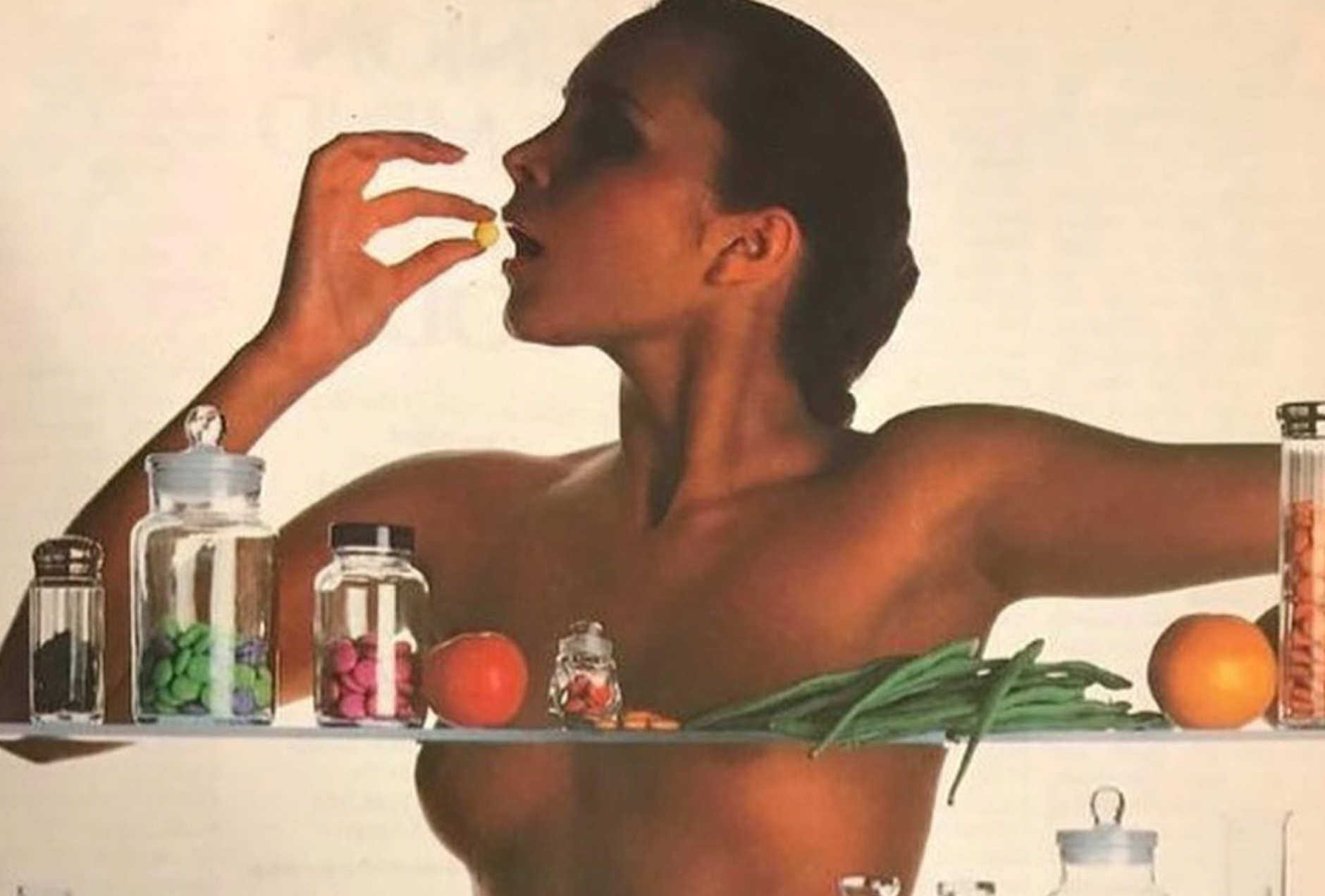
Will taking supplements do anything to help protect us from COVID-19?
There is no strong evidence to suggest these will be beneficial in preventing illness or improving the outcome of COVID-19. There is no evidence to suggest these are harmful when taken as directed and if they make you feel better then that seems reasonable. Just bear in mind their cost as money may better spent on more essential items.
How can we support our healthcare workers at the moment?
Healthcare workers are likely to be working longer hours given increased patients and also staff shortages as we ourselves have to isolate ourselves when we become ill.
The emergency department is going to be hammered with many presentations of COVID-19 in addition to all the other patients needing care for regular illnesses such as accidents and appendicitis etc.
I think it is in everyone’s best interest that patients are seen in the right setting. If you are feeling unwell but don’t think you need to be seen immediately, a call to your GP office can be a good way at minimising the spread of COVID-19 and alleviating the pressure on the hospitals.
There is a new scheme the Australian government is rolling out whereby GPs can perform consultations via the telephone. When assessing patients with a respiratory virus, we can safely manage most patients over the telephone, if we are unsure, we can schedule an examination or advise presentation to hospital. This is quite a sensible option as it limits the exposure of the surgery to Coronavirus; GP surgeries are another place where the most vulnerable patients visit for their other health conditions. GPs can also follow up on patients in isolation looking out for changes in their condition and also their mental health. This is going to be a difficult few months for us all and we need to look out for each other.



